Senator Cortese Newsletter: Together For Earth Day And Each Other

Dear Neighbors,
We embrace the spirit of renewal that April brings. This month, we celebrate Earth Day, a reminder of our shared duty to protect our planet. In the "Community Updates" section below, you'll find information about a fun Earth Day celebration on April 13 in Saratoga. But that's not all: We've included exciting and meaningful events in every major city within Senate District 15: San Jose, Campbell, Cupertino, Saratoga, and Los Gatos. Also, be sure to explore the "State and Local Resources" section for accessible resources in these cities. If you have an event or news item you'd like to suggest for this newsletter, please let us know here.
As we conclude the Christian Easter Lent season on March 31, we also note that April marks the end of Ramadan, a time of fasting, prayer, and community for our Muslim neighbors. We appreciate the values of compassion, charity, and gratitude promoted by all the world’s major religions.
As always, my team and I are here to serve you. We encourage you to reach out with your ideas and concerns, or to share how you plan to make a difference this April. Please get in touch with me at Senator.Cortese@senate.ca.gov.
Warmly,
Senator Dave Cortese

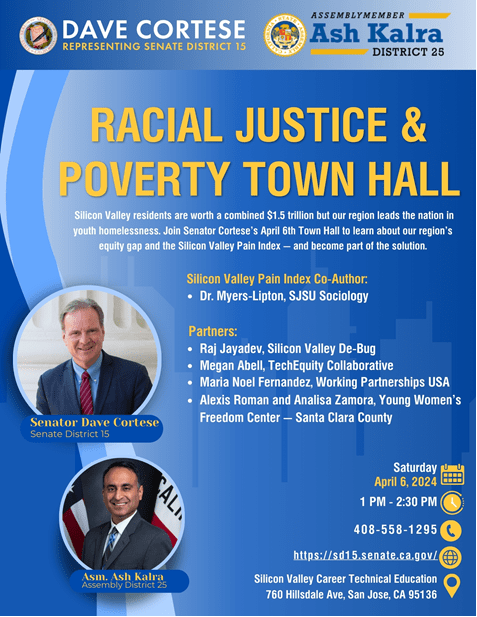
Join My Town Hall on Racial Justice & Poverty
WHERE: Silicon Valley Career Technical Education Auditorium, 760 Hillsdale Ave, San Jose, CA 95136
WHEN: Saturday, April 6th, 1:00pm – 2:30pm
PARKING: Free, on-site parking will be available
You’re invited to a town hall on racial justice and poverty in Santa Clara County with me, Assemblyman Ash Kalra (Assembly District 25), and an exceptional panel.
Last year, the Human Rights Institute at San Jose State University (SJSU) released its fourth annual Silicon Valley Pain Index. The report is full of startling findings, including that Silicon Valley residents are worth a combined $1.5 trillion, but the San Jose region leads the nation in youth homelessness. SJSU Professor Scott Meyers-Lipton will present key takeaways highlighting inequities in the Economy, Workforce Development, and Criminal Justice.
Local leaders from the Young Women’s Freedom Center—Santa Clara County, Silicon Valley De-Bug, Working Partnerships USA, and the TechEquity Collaborative will join us to discuss how they are bridging the equity gap.
Click HERE to register. Please note that seating will be available on a first-come, first-served basis. For more information, don't hesitate to get in touch with Zachary Contini at 408-558-1295 or Zachary.contini@sen.ca.gov.
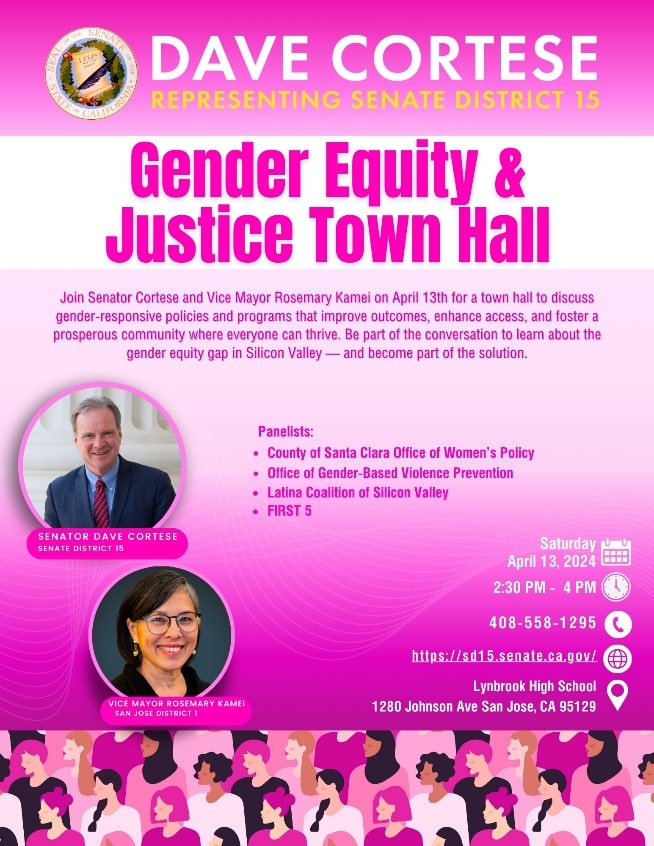
Join My Town Hall on Gender Equity and Justice
WHAT: Town Hall on Gender Equity & Justice in Santa Clara County
WHERE: Lynbrook High School Auditorium, 1280 Johnson Ave., San Jose, CA 95129
WHEN: Saturday, April 13th, from 2:30pm — 4:00pm
PARKING: Free, on-site parking will be available
Join me, San Jose Vice Mayor Rosemary Kamei, and an exceptional panel for a Town Hall on Gender Equity & Justice in Santa Clara County. Our discussion will focus on three critical areas: enhancing childcare access and affordability, advancing gender equity in the workforce, and addressing intimate partner violence.
We'll explore gender-responsive policies and programs designed to improve outcomes, increase access, and cultivate a thriving community where everyone has the opportunity to succeed. Join our town hall to understand the challenges in these areas and to contribute to developing solutions that bridge the gender equity gap.
We’ll be joined by the County of Santa Clara Office of Woman’s Policy, Office of Gender-Based Violence Prevention, Latina Coalition of Silicon Valley, and FIRST 5.
Click HERE to register.
Seating will be available on a first-come, first-served basis. For more information, please get in touch with Estefany Meza at 408-558-1295 or Estefany.Meza@sen.ca.gov.


Senator Cortese takes his Oath of Office to join the California Transportation Commission.
I'm thrilled to announce my recent appointment to the California Transportation Commission (CTC) by Senate President Pro Tem Mike McGuire and my Senate colleagues. This opportunity opens doors for us to significantly influence the future of California's transportation landscape, focusing on enhancing connectivity and safety. My experience as Chair of the Senate Transportation Committee, along with my leadership role at the Bay Area’s Metropolitan Transportation Commission (MTC) and a 20-year member of the Valley Transportation Authority (VTA) in Santa Clara County, has provided invaluable insights into the complexities of transportation in California. I am particularly eager to apply this knowledge as we push forward with my Senate Bill (SB) 915, the Autonomous Vehicle Service Deployment and Data Transparency Act, which will empower local governments to oversee the deployment of autonomous vehicles (AVs), prioritizing public safety and local governance.
SB 915 is already capturing attention statewide — read about it in the "In The News" section below. Currently, the California DMV and the California Public Utilities Commission unilaterally authorize the deployment of AVs over the safety concerns of local governments. Law enforcement can’t issue traffic violations to driverless vehicles, noncompliant AVs have delayed emergency responders, and in San Francisco alone, hundreds of accidents have already dogged driverless “robotaxis.”
But the tide is changing. In recent weeks, the cities of Oakland and Los Angeles and the counties of San Francisco, Los Angeles, and San Mateo have endorsed SB 915. My bill will ensure balanced oversight between driverless and conventional vehicles, making local input a cornerstone of the safe introduction of autonomous vehicles.
Also, in March, I joined my fellow legislators to unveil the "Working Together for a Safer California" plan. This bipartisan effort tackles the pressing issues of retail theft and fentanyl through a holistic approach, including prevention, treatment, and reinforced support from law enforcement. Inspired by my involvement in SB 10, Melanie’s Law to stop youth fentanyl overdoses, and my SB 553, which helped ensure workplace safety, this plan is dedicated to safeguarding Californians from violence and the harmful effects of fentanyl. Together with Senate President Pro Tem Mike McGuire and bipartisan colleagues, we are committed to enhancing the safety and well-being of all Californians.

Want us to highlight your event? Enter the date and description here.
Campbell
Hop Into Spring at Campbell’s annual Bunnies & Bonnets Parade!
Saturday, March 30, at 11:00am in Downtown Campbell. Join the 23rd annual Bunnies & Bonnets Parade. This cherished event promises marching bands, dancers, animals and more, creating a perfect family outing. Held rain or shine. The parade starts at the VTA Light Rail tracks and makes its way along Campbell Avenue to Third Street.

Cupertino
Join the Earth & Arbor Day Celebration in Cupertino!
Saturday, April 20, 2024, from 11:00am to 3:00pm. Enjoy a day filled with interactive activities, live entertainment, and food from local trucks. Learn about environmental solutions in a fun, family-friendly setting. Don't miss this opportunity to connect with your community and the planet! At Library Field Park. 10400 Torre Ave STE 4, Cupertino, CA 95014.

Los Gatos
Los Gatos Creek Trail Clean-Up Event: Join Us and Make a Difference!
Saturday, April 13, 2024, from 10:00am to 11:30am. Get involved in community service with the Los Gatos Kiwanis Club and the Key Club from Los Gatos High School! We're meeting up for a trail clean-up at the Old Forbes Mill Parking Lot behind 55 Church St. Help us keep our trails pristine. Supplies like garbage bags and gloves will be provided. Enjoy complimentary light snacks and coffee! For more details, visit lgkiwanis.org.
San Jose
Explore the Creative Pulse of San Jose at South First Fridays
Friday, April 5, 2024 - 5:00pm to 9:00pm. Delight in an evening of art, culture, and community interaction with nearly 20 galleries, shops, bars, and even a yoga studio. Free and open to all every first Friday of the month, immerse yourself in the vibrant art scene of San Jose's SoFA District during this monthly art walk. SoFA District (San Jose), South First Street and William Street, San Jose.
Saratoga
Blossom Day Out: Spring into Fun at the 2024 Saratoga Blossom Festival!
Saturday, April 13, from 10:00am to 4:00pm. Celebrate spring's arrival with the city of Saratoga at the Heritage Orchard and Saratoga Civic Center. This cherished community event, free and open to all, brings together a delightful mix of antique cars, arts and crafts, and live music. Engage in various activities suitable for every age, savor treats from gourmet food trucks, and enjoy the colorful tradition revived by the Saratoga Historical Foundation. 13777 Fruitvale Avenue, Saratoga, CA. For more details, visit saratogahistory.com or call 408-867-4311.
Celebrate Earth Day at Montalvo's Community Celebration
Saturday, April 13, from 11 a.m. to 3 p.m. Join a vibrant Earth Day celebration at Montalvo. Free entry with RSVP, and parking at West Valley College includes shuttle service. Enjoy food trucks, workshops, performances, and more on Montalvo's beautiful grounds. There's something for everyone, from art installations to dance lessons and environmental workshops. Don't miss out on the chance to connect with nature and community! No on-site parking. Free parking and shuttle service from West Valley College will be available throughout the day. 14000 Fruitvale Ave, Saratoga, CA 95070. For more details, visit Montalvo's website.

Santa Clara County
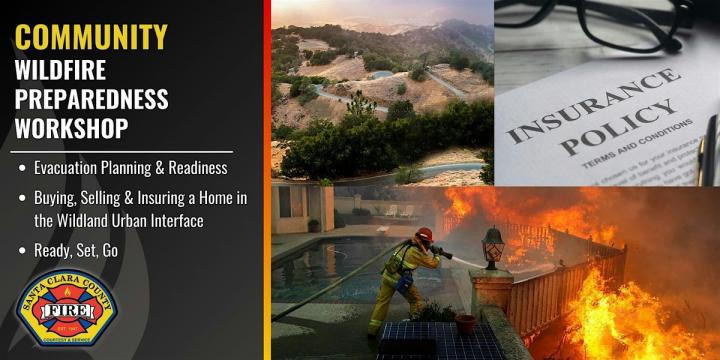
Get Ready for Wildfire Season: Community Preparedness Workshop 2024
Wednesday, May 8, 6:00pm to 8:00pm. Prepare for wildfire season with the Santa Clara County Fire Department and the California Department of Insurance. Learn crucial tips on making your home resilient, evacuation planning, and navigating insurance processes in wildfire-prone areas. This vital workshop is designed to keep you and your property safe. This training class is open to individuals who live or work within the communities served by the Santa Clara County Fire Department: Campbell, Cupertino, Los Gatos, Los Altos, Los Altos Hills, Monte Sereno, Saratoga and the unincorporated surrounding areas. Los Altos Hills Town Hall, 26379 Fremont Road, Los Altos Hills.
Become a Community Hero: Join the Spring CERT Academy!
The Santa Clara County Fire Department is now accepting registrations for its Community Emergency Response Team (CERT) Spring Academy. Starting this April at the City of Los Altos Community Center, the academy offers both in-person and online classes on Tuesdays and Thursdays from 6:00 p.m.-9:00 p.m., culminating in a hands-on skills day and graduation on Saturday, May 4, from 8:30 a.m. to 1:00 p.m. A $35 fee includes essential Personal Protective Equipment. Open to residents and workers in specific Santa Clara communities, ages 16 and up. Click here for more information and to register.

Volunteer at First Friday Beautification Days
Friday, April 5, 2024 | 9:00 AM to 12:00 PM. Lend a hand in preserving the beauty and history of Santa Teresa - Bernal-Gulnac-Joice Ranch. Join Friends of Santa Teresa Park for a morning of community service, which includes gardening, barn maintenance, and caring for the historic house. Discover the rich history of the land while contributing to its upkeep. Minimum volunteer age: 8. Release forms are required for children under 14. Join us to make a difference in your community! Register here. 372 Manila Dr, San Jose, CA 95119.

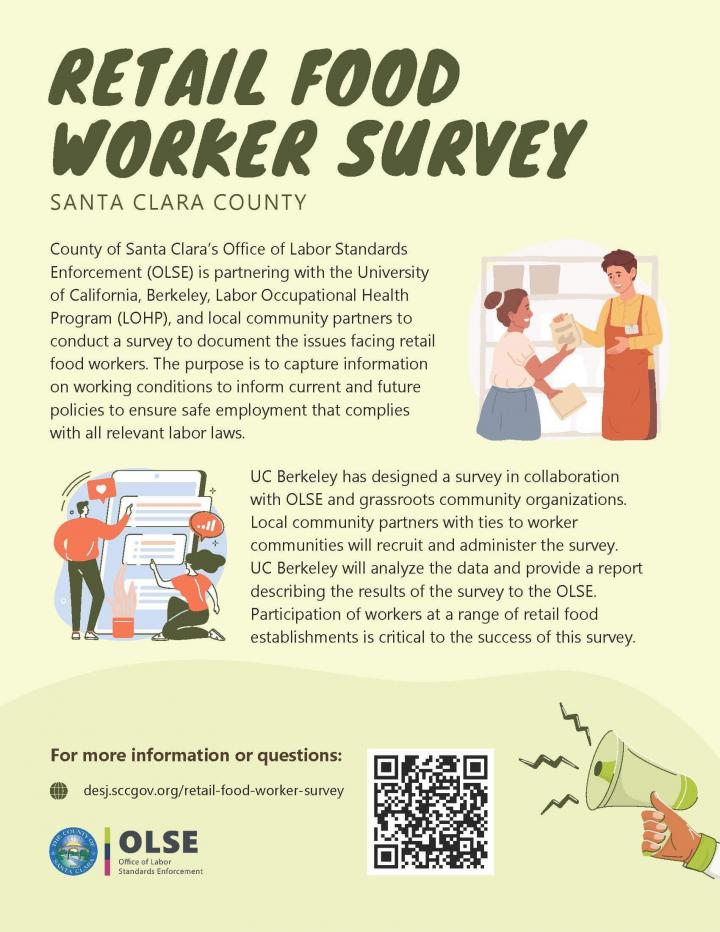
Take Part in the Retail Food Worker Survey
Santa Clara County's Office of Labor Standards Enforcement (OLSE), in partnership with UC Berkeley's Labor Occupational Health Program and local organizations, invites retail food workers to participate in a vital survey. This effort seeks to understand your experiences in the industry, aiming to ensure safe working conditions and adherence to labor laws. Your input will help shape future initiatives to better support workers and businesses. Don't miss this chance to contribute to meaningful change in your workplace. Click here or See bar code below.
Become a Certified Family-Friendly Workplace in Santa Clara County
Boost your business's reputation and productivity by joining the Family-Friendly Workplace Certification Program (FFWCP)! This initiative celebrates businesses that support employees with pregnancy and parental leave, lactation accommodations, and work-family balance. It's free for all Santa Clara County employers and offers exclusive access to expert advice and a digital seal for marketing. Don't miss our virtual training on March 29, 2024, from 10:00am to 11:30am to learn more. Register here and visit Santa Clara County’s website for complete details.
Santa Clara Family Health Plan (SCFHP) Scholarship Program
Are you pursuing a career in healthcare? The Santa Clara Family Health Plan is excited to announce our 25th Anniversary Health Career Scholarship Program, designed to support SCFHP Medi-Cal members. This initiative offers up to $5,000 per year to SCFHP Medi-Cal members pursuing healthcare degrees/certifications at select local institutions, including San José State University, Evergreen Valley College, Mission College, West Valley College, San José City College, and more. Applications for Fall 2024 are now open. For more details and to apply, visit scfhp.com/scholarship.
Join the County Parks Trail Watch and Make a Difference!
Love the outdoors? Become a Trail Watch volunteer for Santa Clara County Parks! As the "eyes and ears" on the trails, you'll provide vital information to park visitors and assist in emergencies. Whether you prefer hiking, biking, horseback riding, or motorcycle patrol, there's a spot for you. Visit the SCC Volunteers website, call (408) 918-4930 or email volunteer@prk.sccgov.org.

The First Corazon Care Campus to open on April 20
Thursdays, 5:30 p.m. to 7:30 p.m. Saturdays, 8:30 a.m. to 11:30 a.m. I’m thrilled to introduce the opening of the Corazon Care Campus on April 20, a secure and welcoming recreational environment for young children with Autism Spectrum Disorder (ASD) in Santa Clara County. Spearheaded by the "Corazon Care" Advisory Board, which I sit on alongside regional leaders in special education, the campus will meet the unique needs of young children with ASD. The indoor campus will feature sensory toys, play areas, and amenities tailored to various sensory preferences, promoting these children's physical and emotional well-being and supporting their families and caregivers. Children must be supervised at all times. No registration needed. Located at the Centennial Recreation Center Multipurpose Room. 171 W. Edmundson Avenue, Morgan Hill, 95037.

NBC Bay Area: South Bay lawmaker introduces bill aimed at preventing fentanyl poisoning deaths among children
The Mercury News: Baby Phoenix’s fentanyl overdose death inspires state legislation to protect opioid’s youngest victims
Los Angeles Times: Waymo to launch robotaxi service in Los Angeles, but no freeway driving — for now
Sacramento Bee: Newsom stays silent on Cal-OSHA staffing crisis as legislators and advocates call for action
KTVU Fox 2: California 'Waymo' bill aims to give cities more authority over self-driving car companies
KTVU Fox 2: California bill seeks to speed up construction of interim housing
SacBee: Senate Transportation Chair Opens Up About Autonomous Vehicles


It was great to talk about state funds for major LA transportation projects with Los Angeles District 1 Supervisor Hilda Solis. She is a longtime supporter of worker’s rights, good jobs and workplace safety, and served as U.S. Secretary of Labor under President Obama.

It was great to meet Hadi Ahmadi Aval from New York Life, who has worked as a financial advisor in our district for many years, during a legislative visit. Hadi and I support SB 263 (Dodd), which will extend consumer protections for individuals investing in annuities, including numerous vulnerable seniors. This bill will safeguard people from being misled or directed towards unsuitable products by unethical insurance agents. SB 263 is pending before the Governor.

It was a pleasure to welcome representatives from the Special Olympics on the Senate floor. I’m honored to support these incredible athletes who teach us all about courage and strength.

My district representative, Estefany Meza, joined the annual Berryessa Citizens Advisory Council “Citizen of the Year” award. As a past recipient, I was proud this year to recognize Eric Pennington with a Senate resolution. This event is an excellent reminder of our community's strength and spirit.

I was honored that the California Judges Association and its President, the Honorable Judge Erica R. Yew, awarded me the Scales of Justice award! I’ve partnered with their organization on pivotal legislation protecting youth involved in foster care and the juvenile justice system. (My SB 9, SB 383, SB 384). Thank you to Assemblymembers Ash Kalra, Steve Bennett, and Senator Steven Bradford for joining me in this honor.

I joined a dynamic panel with the Santa Clara County School Boards Association to discuss K-12 education. Despite our budget challenges, we absolutely need to protect K-12 education funding. Our students need quality education to springboard into great careers. It was a pleasure to join Assemblymember Gail Pellerin and Senators Aisha Wahab and John Laird as panelists at the forum.

A big congratulations to the new Bill Wilson Center at Westminster Presbyterian Church! My district representative, Estefany Meza, joined Bill Wilson Center’s CEO, Josh Selo, in announcing an exciting new chapter for an organization that does so much to prevent, shelter, and end youth and family homelessness in our region.

My district representative, Zach Contini, joined Paul Lorenz, CEO of Santa Clara Valley Medical Center, and Supervisor Cindy Chavez for a ribbon-cutting ceremony for HomeFirst Shelter. We celebrate a new shelter and one new pathway to recovery, stability, and hope for those living on the street.

Congratulations to San Jose Clean Energy on celebrating its fifth anniversary! This Community Choice Aggregator, established by the city of San Jose, helps convert the city to a clean energy grid, giving people a choice in their energy source.

I joined Senator Steve Padilla and the Silicon Valley Leadership Group for an engaging discussion about data centers. My SB 1298 will allow for the expansion of data centers to grow our state technology sector and protect California’s economy.
City of San Jose
- Alviso and Biebrach Pool Information
- Apply for a Building Permit
- Buy Happy Hollow Park & Zoo Tickets
- Covid-19 Resources
- Food and Family Resources
- Free Junk Pickup
- Housing Resources
- Immigration and Community Resources
- Job Training
- Make a payment for Utilities, Recycling & Garbage
- Pay or Contest a Parking Citation
- Pet Licensing
- Register your Business or Rental
- San Jose Public Library
- Sign your kids up for Preschool
- Sign up for Recreational Activities
City of Campbell
- Building Permits
- Camps
- Careers
- Community Center Pool
- Email the City
- Recreation Classes
- Parks and Recreation
- Preschool
- Summer Camps
- Skate Park
- Volunteer
- Youth Activities
City of Cupertino
- Building Permits
- Business License
- Commission Membership
- Cupertino Volunteer
- Dog & Cat Licenses
- Job Openings
- Outdoor Activities
- Parks
- Planning and Building
- Preschool
- Public Safety
- Recreation Classes and Activities
- Residential Parking Permit
- Schedule a Building Inspection
- Schools
- Senior Center
- Senior Citizen Utility Tax Exemption
- Teen Commission
- Utilities
City of Los Gatos
- Arts and Culture
- Building Permit
- Business Licenses
- Clerk Administrator
- Contact
- Code Compliance
- Community Development
- Employment Opportunities
- Events and Activities
- Human Resources
- Jobs
- Parks and Public Works
- Parking & Traffic
- Planning Commission
- Police Services
- Town Council
- Town Manager
- Staff Directory
City of Saratoga
- Business License
- Code Violations
- Home Renovation Design Review
- Issues (Potholes, Street Lights, Etc.)
- Parks and Public Works
- Public Safety
- Tree Removal Permit
- Missed Garbage Pickup
- Volunteering
Santa Clara County
- Birth and Death Registration
- Domestic Violence Resources (Hotline call 800-799-7233)
- Resources for Homeless Young People: Bill Wilson Center
- Center for Employment Training / Job Counseling, Financial Support and Job Board
- Free/Low Cost Healthcare for Families and Children
- Childcare Resources
- Resources for Families Struggling with Mental Illness
- Free Legal Help: Family Law, Civil Rights, Employment Law
- Public Health Pharmacies
- Free Healthcare for Qualifying Families
State Assistance

- CalFresh / SNAP (Supplemental Nutrition Assistance Program
- COVID Sick Leave Navigator
- Food Assistance
- Mortgage Relief
- Protection against eviction and help with payments for rent and utilities
- Ways to Apply for Medi-Cal
- Find Affordable Health Insurance
- Find Mental Health Services
- Suicide Prevention and Resources (Suicide Hotline – Call 988)
- Domestic Violence Restraining Orders
- Water Bill Assistance
Auto
- Driver’s License / ID Card Application
- Register Your Vehicle / Register Your Boat
- Apply for a FasTrak Toll Device
Business Assistance
- GO-Biz Governor's Office of Business and Economic Development Free consultation for identifying tax incentives, site selection, regulatory or permitting compliance assistance, foreign direct investment and exports.
Consumer Protection
Jobs and Unemployment
- Search Job Listings
- Get a State Job
- File for Unemployment
- Locate Your local Worker’s Comp office
- Services for Veterans
- Services for Older Workers
Road Conditions
- Look up by Highway / Look up by Map / Call 511
Seniors
State and Federal Legislation
Travel
- Amtrak
- Reserve a State Park Campsite
- BART Bay Area Rapid Transit
- VTA Valley Transportation Authority
- All-In-One Transit Card: Get a Clipper Card
Voting
As always, please feel free to contact me with any questions, comments, or concerns. I can be reached at senator.cortese@sen.ca.gov.